Foreign Bodies
Nose (mostly kids): Look with nasal speculum and the end of flex scope to confirm. For management, it’s safest just to take to the OR, remove under mask anesthesia. Foreign bodies in the nose usually need to be taken care of before sending patient home as they are at risk of aspiration. It is helpful to decongest the nose prior to retrieving the foreign body.
FB in aerodigestive tract: often just sensation secondary to mucosal irritation. History is very helpful. If the patient reports improving symptoms and is tolerating PO intake you will not likely find a foreign body. If their symptoms are not improving or if things are getting worse, you should keep looking until you find something. Scope in ER—fishbones, toothpicks, etc. often get lodged in the vallecula and patient will be able to localize pain well. Use hurricane spray, and try to remove with forceps (McGill forceps are often helpful) with scope in place to guide you. If your exam only shows edema and erythema it is possible that the foreign body could be buried in the mucosa. Further down the aerodigestive tract it is more difficult for patients to localize, more difficult to visualize and more controversial for management. May get a Neck/ chest PA/ lateral, may get barium swallow (plain films see fishbones less than 50% of the time whereas a CT scan is close to 100% sensitive but usually not necessary).
Angdioedema
This disease occurs as one feature of an anaphylactic or anaphylactoid reaction. Drugs such as acetylsalicylic acid and angiotensin-converting enzyme (ACE) inhibitors are known to precipitate an attack. With ACE inhibitors, bradykinin appears to have a major pathogenic role. By contrast, the forms caused by a C1 esterase inhibitor (C1-INH) deficiency are much less common. Angioedema due to C1-INH deficiency may be hereditary or acquired. Patients present with sometimes massive facial swelling that is most pronounced in the periorbital region but also affects the lips, tongue, base of tongue, and supraglottic structures.
Assure airway stability by examining the airway with a scope. Administer steroids, H1 blockers (Benadryl), and H2 blockers. Epinephrine may be administered if severe or progressing. Humidified Oxygen. Elevate head of bed. Usually resolves quickly in ER, but requires admission to ICU if there is any question of airway stability. Severe cases may require intubation or emergent tracheotomy.
e-MEDICINE Angioedema Overview
Epiglottitis
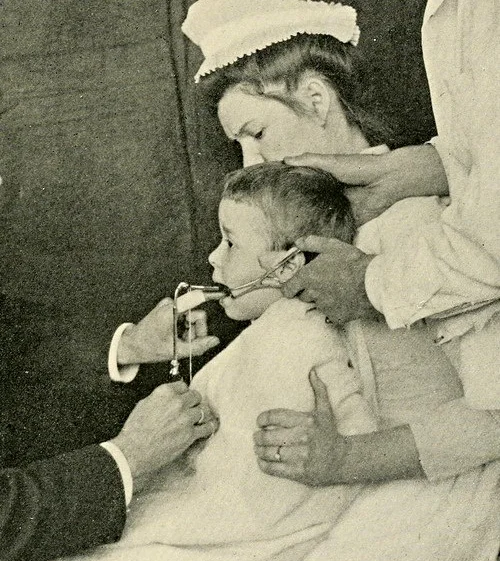
Management same as airway and other infections above except adults and children treated differently. Adults can be scoped with concerns of the epiglottis without issue, children should be done more cautiously as it can cause laryngospasm. Since the widespread implementation of a conjugate vaccine for Haemophilus influenzae type b (Hib) nearly 2 decades ago, the incidence of epiglottitis has significantly declined in children. The clinical triad of the ‘‘three
Ds’’ (drooling, dysphagia, and distress) is a classic presentation. A viral prodrome and cough are seldom observed with acute epiglottitis and are more often witnessed in association with croup. Patients generally appear toxic and anxious. Often they assume the ‘‘sniffing position,’’ with the head hyperextended and nose pointed superiorly in an effort to maintain a patent airway. Vocalization is quite painful, and the patient may speak with a ‘‘hot potato’’ or muffled voice.
Lateral neck films may demonstrate the classic thumb sign, indicative of the severe edema involving the epiglottis. The poor sensitivity and specificity of plain films limits the utility of this imaging study. The larynx can usually be safely and accurately visualized with flexible laryngoscopy. Contrasted CT scan of the neck may also indicate the presence of epiglottic edema and possibly phlegmon or abscess in the epiglottis or the base of tongue.
Intubation is usually unavoidable in a true case of epiglottitis in the pediatric patient. Securing the airway should be accomplished immediately in a controlled setting (most deaths occur in prehospital settings). Given the short natural history of the disease, a tracheotomy is usually not necessary. ABX treatment should involves a third-generation cephalosporin. With prompt treatment most patients can be extubated after the regression of inflammation, usually 1-3 days after intubation.
The incidence of epiglottic abscesses appears to be increasing with the rise in acute epiglottitis in adults.
e-MEDICINE Pediatric Epiglottitis Overview
e-MEDICINE Adult Epiglottitis Overview
DISCLAIMER: The content of this Website is not influenced by sponsors. The site is designed primarily for use by qualified physicians and other medical professionals. The information contained herein should NOT be used as a substitute for the advice of an appropriately qualified and licensed physician or other health care provider. The information provided here is for educational and informational purposes only. In no way should it be considered as offering medical advice. Please check with a physician if you suspect you are ill.