Chapter 2
MYRINGOPLASTY
Raleigh O. Jones
Confusion has existed for many years regarding the nomenclature used to describe surgery on the tympanic membrane (TM), middle ear, and ossicular chain. Wullstein’s classic classification system (types IV) was based on the relative position of the TM to the other middle ear structures including the ossicles and inner ear membranes.1 This description was developed prior to the introduction of many of the procedures and prostheses that are used so commonly today in middle ear surgery, so its ability to adequately describe current surgical techniques is limited. Consequently, the term tympanoplasty by itself is not adequately descriptive, simply indicating some sort of reconstructive surgery on the TM or middle ear. It is therefore necessary for the surgeon to use further descriptive terms in addition to the term tympanoplasty to communicate effectively which procedures are being described.
The term myringoplasty refers to reconstructive surgery that is limited to the TM. It was actually introduced by Berthold, who successfully closed a TM perforation using a full thickness skin graft in 1878.He was the first to report the use of autologous tissue in an effort to repair the TM; prior to that, several different artificial or animal-based materials were used dating back to as early as 1640.By definition, any manipulation of the ossicular chain is beyond the scope of a pure myringoplasty. Because the term tympanoplasty includes surgery on both the TM and middle ear, however, many cases of myringoplasty are labeled tympanoplasty by surgeons, further adding to the confusion. The terms myringoplasty and tympanoplasty without ossicular reconstruction are synonyms unless other manipulation of the middle ear such as removal of cholesteatoma is included in the tympanoplasty procedure. Within the more limited surgery of the TM, many different approaches to myringoplasty have been described.
PATIENT PRESENTATION
Patients with perforations of the TM may present acutely or with symptoms suggestive of a chronic perforation. Acute perforations are usually the result of acute otitis media with rupture of the TM due to increased pressure in the middle ear, trauma to the ear canal or temporal bone, or sudden pressure changes transmitted to the TM.
The majority of cases of acute otitis media resolve spontaneously with or without medical treatment and without any significant injury to the TM. Certain infections, however, build up sufficient pressure within the middle ear space, which is effectively closed due to eustachian tube blockage, that the flexible TM ruptures, thereby relieving this pressure. This acute event is associated with sudden drainage from the ear that is often both bloody and purulent, and also with an increase in pain followed by a marked diminution of pain. This rupture of the TM effectively releases the infection from out of the skull and away from other fragile and vital structures such as the central nervous system (CNS) and the inner ear. Most cases of acute TM perforations due to infection will heal without surgical treatment over a period from a few days to a few weeks. Resolution of the infection is an important consideration as to whether this healing will occur because a perforation is more likely to remain open if the drainage persists. Treatment of such infections with both systemic antibiotics and aural antibiotic drops is highly recommended. Although not proven, it is believed that thin, atelectatic TMs are more likely to rupture and less likely to heal without surgery than normal membranes. Trauma can produce a tear in the TM either directly, such as a penetrating injury, or indirectly, such as from a shearing movement in bone as seen in a temporal bone fracture. Although any small object could produce a penetrating injury, the cotton- tipped swab is a particularly common offender, because it is used in an attempt to clean or scratch the ear canal and too often finds its way through the TM. These perforations are typically central in location and can be quite large. A discussion of the possible trauma to the ossicles and inner ear is beyond the scope of this chapter, but the perforation will be accompanied by a moderate amount of self- limited bleeding and sudden pain. Temporal bone fractures may present with hemotympanum when the TM is intact or with a perforation and bleeding when the annulus or TM is torn. Longitudinal fractures are particularly prone to tearing the TM, but mixed or transverse fractures may also present in this manner.
Significant changes in pressure in the outer ear may also produce ruptures of the TM. This can be negative pressure, as is seen in injuries that occur while flying in which the cabin pressure is not maintained adequately, or positive pressure such as a slap with a cupped hand to the ear canal, resulting in pushing on the TM. Again, a sudden onset of pain and bleeding accompanied by some degree of hearing loss are usually present. The pain and bleeding usually resolve quickly without treatment, and unless infection develops, no otorrhea occurs and the patient is asymptomatic with the exception of a hearing loss.
Patients with a chronic perforation of the TM usually present with a conductive hearing loss, otorrhea, or both. Nearly all patients with a chronic perforation of their TM have otorrhea to some degree. There is a wide spectrum of the severity of this symptom. Some patients are not able to recall ever having an episode of drainage, whereas other patients have constant drainage of malodorous, discolored material that drains into their conchal bowl, onto their ear lobe, and even onto their upper neck on a daily basis. Between these two extremes, most patients have intermittent drainage that may occur spontaneously or be brought on by getting water in the ear or suffering from an upper respira- tory infection. These infections are typically caused by multiple microorganisms, particularly Pseudomo- nas, Staphylococcus, Proteus, and various anaerobic bacteria. They are frequently resistant to most orally administered antibiotics presumably due to the repeated courses of antibiotics that have been used to treat this condition over the period of the existence of the perforation.
AUDIOLOGIC CONSIDERATIONS
Patients with a chronic TM perforation generally present with a conductive hearing loss. The degree of hearing loss varies significantly among patients, from no detectable loss up to a moderate conductive loss. Among the factors influencing the degree of hearing loss present are the size and location of the perforation, the presence of otorrhea, and the status of the ossicular chain. Other chapters of this book address details of ossicular absence, erosion, or fixation, but with an intact ossicular chain the conductive hearing loss associated with a TM perforation rarely exceeds 35 dB, regardless of the size or location of the hole.
Small perforations may be associated with no significant impairment of hearing. Generally speak- ing, the larger the perforation, the greater the degree of hearing loss. Initially the conductive hearing impairment affects only the very low frequencies, but as the size of the perforation increases, the hearing loss increases and involves more of the middle frequencies.5 Anterior perforations tend to produce smaller hearing losses than their posterior counterparts, presumably due to the exposure of the round window to the effect of sound waves penetrating directly through the perforation and striking the round directly setting up a competing fluid wave within the inner ear. Even large anterior perforations rarely produce greater than 15 dB of conductive hearing loss in the absence of infection or ossicular involvement. In addition to the effect of the exposing the round window directly to the sound waves, perforations also produce hearing loss by diminish- ing the surface area of the TM available to collect the energy in the form of sound waves and then transmit that energy onto the inner ear via the ossicular chain. It is therefore understandable that larger perforations produce a greater degree of hearing impair- ment.
PREOPERATIVE ASSESSMENT
For a patient presenting with a perforation of the TM, the physician should take a thorough history and perform a physical examination. The history should attempt to determine if the perforation is acute or chronic and what if any event precipitated the perforation. Because most acute perforations heal spontaneously with proper medical treatment, determining when the perforation developed is a prime consideration. Ears with acute perforations should be cleaned and examined carefully under a microscope. If edges of the perforation can be seen to be deflected medially into the middle ear, it is desirable to elevate them gently with a suction to prevent squamous epithelium from growing in the middle ear. It is neither necessary nor desirable to treat these acute perforations with antibiotic ear- drops, as many of the currently available drops contain materials that may be ototoxic when ex- posed to the round window. It is indeed desirable to prevent infection, so these patients are advised to keep all water out of their ears and watch for any signs or symptoms that would suggest infection. When infection does occur, treating it aggressively will increase the likelihood that spontaneous healing will occur.
Patients with chronic infection rarely recall when their perforation first developed. Their history should focus on the presence of other factors that may influence eustachian tube function and healing after surgery, as well as on what other attempts have been made to treat this condition. Eustachian tube function is a major factor in determining the ultimate success of tympanoplasty or myringoplasty surgery. Patients with poor eustachian tube function may heal their perforations successfully after surgery, only to be left with a conductive hearing loss equal to or even greater than the loss they had prior to surgery if serous otitis media should develop. Indeed, small perforations may act in a manner similar to a PE tube placed by an otolaryngologist in an ear with poor eustachian tube function and at times should be viewed positively by both patient and surgeon. This is particularly true in children, among whom eustachian tube dysfunction is a common problem. Unfortunately, there are no tests that can predict with a high degree of success the status of the eustachian tube function prior to surgery to close a perforation.In fact, there is evidence that merely closing a perforation may have a beneficial effect on the function of the eustachian tube.The status of the eustachian tube in the other ear gives some indication of the function in the involved ear, but this is not a universally effective predictor either. Though opinions vary, many surgeons prefer not to repair dry perforations associated with minimal hearing loss in children’s ears until the child is 6 or 7 years old, hoping that eustachian tube function will be adequate at that point to yield an air-containing middle ear space with normal hearing after the procedure. Even if the procedure is successful in closing the perforation, recurrence of the perforation is a particular concern in children. Reperforation rates of 10 to 20% have been reported,although Tos and Lau reported reperforation rates in children as low as 4%, although approximately 6% developed serous otitis media significant enough to require PE tube place- ment after successful closure.
Preoperative planning also includes a careful inspection for evidence of cholesteatoma that would require a more extensive surgery to eradicate. Routine imaging of patients with TM perforations is not required, nor justifiable, but circumstances may exist that would make a computed tomography (CT) scan appropriate to evaluate the extent of infection. Among the reasons for preoperative scanning are dizziness, unusual pain, or a suspected intracranial complication. It is important to realize, however, that the presence of infection does not mean that a procedure other than a myringoplasty will be needed to close a perforation.
A serious effort to resolve all active drainage from an ear prior to an operation is an important adjunct to the surgery. Pignataro et alhave confirmed a commonly held belief among ear surgeons that dry perforations are more likely to heal following myringoplasty or tympanoplasty than those with persistent infection. This is particularly true when a myringoplasty is considered because any infection in the middle ear is not addressed by this procedure. Most ears with active drainage can be improved with proper treatment to the point where the drainage stops or is significantly decreased. Careful microscopic cleaning is the first step in this process. Repeated cleaning alone without any other treatment often produces dramatic results, and when combined with appropriate antibiotic treatment usually leaves the patient with a dry perforation ready for surgery. Antibiotic cultures are not routinely obtained, but when the patient does not respond to treatment, these cultures can be helpful in directing further therapy. It is important to remember the possibility of unusual infections, such as with Mycobacterium, in patients who are immunocompromised or who do not respond as expected to treatment. In addition, many of these patients have been treated extensively with antibio- tics, and fungal infections are frequently seen. Cultures may help direct therapy successfully when the usual improvement is not seen with local cleaning and antibiotic drops.
Successful medical treatment of otorrhea has benefits beyond that of improving the success rate of the surgery. Landmarks are more readily visible and the surgery is often accomplished in a shorter period than in ears with active infection. In addition, polypoid, chronically infected, and thickened mu- cosa with or without granulation tissue make the surgery more difficult and increase the possibility of a surgical complication. Still, the presence of active drainage in an ear does not mean that a perforation cannot be successfully closed with a good surgical procedure, although the procedure may need to address more than the perforation itself, including removal of infection from the middle ear and/or mastoid.
Every patient who is a potential candidate for surgery on the TM should have a current audiogram to document for legal purposes any presurgical hearing deficit, but also to provide a valuable piece of information regarding the status of the ossicular chain prior to the operation. This information helps determine whether the patient is a candidate for a myringoplasty or needs formal tympanoplasty.
OPERATIVE PROCEDURES
Many different techniques have been developed over the past 50 years in an attempt to close perforations and several materials have been used for grafting material. Initially, split or full-thickness skin grafts were employed. The material was readily available near the operative site and was inexpensive, autologous, and readily shaped. However, many cases of improper growth of squamous epithelium either within the TM or in the middle ear occurred with this technique, leading to the search for other materials. Vein grafts, perichondrium, cartilage, fat, and homologous dura or fascia have been used,although the most common material used today is temporalis muscle fascia harvested from a small incision behind and slightly above the patient’s ear within the operative field. This fascia is semitransparent and flexible like a TM, and has roughly the same thickness as a TM when properly prepared. In addition, other synthetic materials such as rice paper and dissolvable synthetic collagen (Gelfilm) have been utilized in certain specific situations discussed below.
How and where these materials are placed relative to the remaining perforation also varies from one technique to another. Two of the most common methods for myringoplasty include the underlay and overlay methods discussed in detail in Chapters 3 and 4. These procedures are named according to the position of the graft relative to the remaining anterior TM, although both techniques place the graft medial to the handle of the malleus when the perforation involves the superior half of the TM. The underlay technique also allows good exposure to the middle ear required for tympanoplasty, but for myringoplasty alone this is not needed.
Although the surgical repair of acute perforations is not required to yield good results for closure, it is thought that certain perforations may benefit from surgical manipulation in a limited manner. The desirability of elevating depressed remnants of TM out of the middle ear has already been mentioned. In addition, many surgeons attempt to put a temporary covering over these perforations to aid healing, serving as a scaffold for the TM to grow beneath and also as a barrier to keep infection from migrat- ing into the middle ear from the external ear. A special instance frequently encountered is the acute perforation created surgically when retained PE tubes are removed. It is known that patients who have PE tubes removed that have been in place for 3 years or longer are at significantly greater risk for nonhealing following removal. Patching these perforations acutely at the time of tube removal has been done in an effort to reduce this rate of permanent perforation, although two studies have called the efficacy of this procedure into question.Rice paper has been used and described most extensively for this procedure.
This procedure is generally done in the clinic without any anesthesia. An operating microscope is utilized and the external canal is cleaned. The edges of the perforation are elevated gently with a small suction; then a circular patch approximately 3 mm larger than the perforation is cut from cigarette paper that has been previously sterilized with steam. It is desirable to leave the paper dry when placing it directly on top of the remaining TM, ensuring that the perforation is completely covered. The patch needs to sit directly on the TM. If it is bent slightly and therefore not in direct contact, a small drop of saline can be placed on the paper patch allowing it to conform to the contour of the TM. The patient is then instructed to keep all water out of the ear and to notify you if any discharge occurs. The procedure is nearly painless and should take 5 minutes or less. The patient returns to the office in approximately 2 weeks and the patch is removed under the microscope. The success rate for closure of acute perforations is quite high, with smaller perforations having a nearly 100% success rate and even larger perforations close at a rate of approximately 90%. Gold and Chaffoo17 created acute perforations in guinea pigs and randomized them to treatment with fat myringoplasty, paper patch, or control. They demonstrated healing in 88, 56, and 75% of these groups, respectively. Although statistical significance was not reached in this study, it does demonstrate the expected high rate of spontaneous healing and the safety of these minor procedures in the guinea pig model. Imamoglu et al18 did a similar study in rats where the success rates for small perforations using fat, paper, and control were 95, 94, and 67%, but in larger perforations were 53, 56, and 27% respectively. Subsequent series in humans have confirmed these results. It remains unclear which acute perforations would benefit from patching, although it seems as if larger perforations at higher risk for nonhealing may be considered good candidates for this procedure.
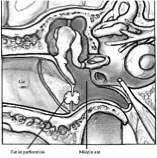
Gelfilm has been used in a similar manner as the paper patch. It has the added advantage of being self-dissolving and therefore does not need to be removed later, a particular advantage in children who may not tolerate this manipulation in the clinic without anesthesia. Chronic perforations can also be closed through a simple myringoplasty technique without the flaps and extensive exposure required for an underlay or overlay tympanoplasty. Many different substances have been used, but the fat myringoplasty has been utilized and studied extensively for 40 years. It has also been used for bilateral TM perforation repair in children with a 91% success rate reported.19 Although some variations in the technique exist, it is important to manipulate the TM to create a fresh surface to which the fat graft adheres. This requires anesthesia of some sort. Although various local anesthetics have been used, a brief general anesthetic is preferred in most cases. The ear canal is thor- oughly cleaned under the microscope and then the edges of the perforation are ‘‘freshened.’’ This is an extremely important part of the procedure and is accomplished by using a sharp instrument or needle to puncture the TM just lateral to the edge of the perforation removing approximately 1 mm of tissue circumferentially around the perforation. This en- larges the perforation somewhat, so it is desirable to remove the minimal amount of tissue necessary to get back to a fresh edge. Numerous studies have shown that the smaller the perforation, the greater the success of this technique, so it is important not to remove any more TM than necessary. The fat is harvested from any site, but generally the ear lobe is readily accessible to the field and fat is readily available. A single piece of Gelfoam (Upjohn Laboratories, Kalamazoo, MI) is placed in the middle ear. A piece of fat just larger than the freshened perforation is harvested and then placed in the perforation in a hourglass shape, with a small amount of the fat protruding through the perforation into the middle ear and a small amount extending just lateral to the TM.20 It is important that the fat is lodged in the perforation and stays firmly in that position (Fig. 21). Generally, a small amount of Gelfoam is placed lateral to the graft in the medial ear canal, although this is not absolutely essential.The patient is instructed to keep all water out of the ear until seen back in the office in approximately 2 to 3 weeks. The success rate for small perforations is quite good ranging from 76 to 92%,21 23 but the success rate for larger perforations ( /4 mm) is poor, approximately 30%.
Even at this low success rate the procedure is so quick, safe, well tolerated, and relatively inexpensive that it is often desirable to try this approach first, with the patient’s under- standing that if it is not successful, it will be followed with a formal tympanoplasty later, which should accomplish a greater than 90% success rate for closure. It needs to be emphasized that this procedure is appropriate only for completely dry perforations where there is no concern for cholesteatoma and where preoperative audiometry reveals no suggestion of an ossicular problem. Studies have shown that attempts at closing perforations with active or recent drainage carry a very low success rate, so this procedure is not recommended in those circumstances.
AlloDerm (LifeCell Corporation, Branchburg, NJ) has also been used in a similar fashion to close small perforations in adults under local anesthesia in the office with good success. The graft should be 1.5 times as large as the perforation, because it is placed onto the TM covering after it is rimmed and a small amount of the outer squamous epithelium around the perforation is removed, leaving a denuded segment of TM adjacent to the perforation. The AlloDerm is then gently pressed onto the perforation, and is then covered with Gelfoam soaked in antibiotic drops (Fig. 22A,B). The ear is kept clean and dry for 6 weeks. Healing has been reported in 86% of cases when small perforations that are dry and stable are treated.
RESULTS
Simple myringoplasty techniques as described in this chapter are highly successful when utilized in the correct circumstance. One- and 2-year follow-up success rates of 80 to 90% have been reported, although some recidivism is reported in children with longer follow-up. Gross et al24 nicely summarized the benefits of myringoplasty (over formal tympanoplasty) when utilized in the proper setting:
Figure 2.1: Fat myringoplasty
Figure 2.2: Alloderm myringoplasty
- Minimal manipulation of the middle ear mini- mizing the risk of operative injury
- Relative simplicity of the procedure.
- Decreased operative and postoperative morbidity.
- Little postoperative care or manipulation is needed, which is particularly important in children
- Decreased operative and recovery time, resulting in decreased cost.
- Bilateral procedures are possible at the same sitting
Because of these real benefits, this procedure should be considered in all patients who present with a small, dry perforation without concern about cholesteatoma or ossicular problems.
REFERENCES
1. Wullstein H. Theory and practice of tympanoplasty. Laryngoscope 1956;66:10761093.
2. Berthold E. Uber myringoplastik. Medicinisch-Chuur- gisches Central-Blatt 1879;14:195207.
3. Guthrie D. The history of otology. J Laryngol 1940;55:473494.
4. Banzer M. Disputatio de Audiotione Laesa. Wittebergae, 1640. Cited by House H. XVIII Wherry Memorial Lecture: otology in orbit. Trans Am Acad Ophthalmol Otolaryngol 1963;67:233259.
5. Tonndorf J, McCardle F, Kruger B. Middle ear transmission losses caused by tympanic membrane perforations in cats. Acta Otolaryngol 1976;81:330336.
6. Todd NW. There are no accurate tests of eustachian tube function. Arch Otolaryngol Head Neck Surg 2000;126:10411042.
7. Tos M. Tubal function and tympanoplasty. J Laryngol Otol 1974;88:11131124.
8. Kessler A, Potsic WP, Marsh RP. Type 1 tympano- plasty in children. Arch Otolaryngol Head Neck Surg 1994;120:487490.
9. Tos M, Lau T. Stability of tympanoplasty in children. Otolaryngol Clin North Am 1989;22:1528.
10. Pignataro L, Grillo Della Berta L, Capaccio P, Zaghis A. Myringoplasty in children: anatomic and func- tional results. J Laryngol Otol 2001;115:694698.
11. Goodhill V. Articulated polyethylene prosthesis with perichondrial graft in stapedectomy. Rev Laryngol (Bordeaux) 1951;82:305320.
12. Tabb HG. Closure of perforations of the tympanic membrane by vein grafts: a preliminary report of 20 cases. Laryngoscope 1960;70:271286.
13. Storrs L. Myringoplasty with the use of Fascia Grafts. Arch Otolaryngol 1961;74:4549.
14. Yetiser S, Tosun F, Satar B. Revision myringoplasty with solvent-dehydrated human dura mater (Tuto- plast). Otolaryngol Head Neck Surg 2001;124:518521.
15. Nichols PT, Ramadan HH, Wax MK, Santrock RD. Relationship between tympanic membrane perfora- tion and retained ventilation tubes. Arch Otolaryngol Head Neck Surg 1998;124:417419.
16. Pribitkin EA, Handler SR, Tom LW, Potsic WP, Wetmore RF. Ventilation tube removal: indications for paper patch myringoplasty. Arch Otolaryngol Head Neck Surg 1992;118:495497.
17. Gold SR, Chaffoo RAK. Fat myringoplasty in the guinea pig. Laryngoscope 1991;101:15.
18. Imamoglu M, Isik AU, Acuner O, Harova G, Bahadir O. Fat-plug and paper-patch myringoplasty in rats. J Otolaryngol 1998;27:318321.
19. Mitchell RB, Pereira KD, Younis RT, Lazar RH. Bilateral fat graft myringoplasty in children. Ear Nose Throat J 1996;75:655656.
20. Mitchell RB, Pereira KD, Lazar RH. Fat graft myr- ingoplasty in children: a safe and successful day-stay procedure. J Laryngol Otol 1997;111:106108.
21. Terry R, Belline M, Clayton M, Gandhi A. Fat graft myringoplasty: a prospective trial. Clin Otolaryngol 1998;13:227229.
22. Ringenberg J. Closure of tympanic membrane per- forations by the use of fat. Laryngoscope 1978;88:982983.
23. Althaus S. ‘‘Fat plug’’ myringoplasty: a new techni- que for repairing small tympanic membrane perfora- tions. In: Brackman DE, ed. Otologic Surgery. Philadelphia: WB Saunders; 1994:112119.
24. Gross CW, Bassila M, Lazar RH, Long TE, Stagner S. Adipose plug myringoplasty: an alternative to formal myringoplasty techniques in children. Otolaryngol Head Neck Surg 1989;101:617620.