MATCH STATISTICS
Otolaryngology has always been a very competitive residency to match into. Yet, each year’s individual statistics can vary dramatically. In 2018, there were 333 applicants (299 MD Seniors) for 315 positions, which provides a match rate of approximately 95%, a remarkably high number for a surgical subspecialty. However, NRMP Match data reveals that in 2020 there were 505 applicants for 350 spots, which offers a match rate of 69%. Specifically, there were 421 MD Seniors (non-graduated allopathic medical students) who applied and 310 MD Seniors who matched for an MD Senior match rate of 73.4% with only 2 unfilled spots. While these numbers can seem daunting, they can be overcome with good planning and proper preparation.
While there is a lot that goes into a residency application, a study by Hauser et al. (2017) suggested that applicants who were successful at matching into an Otolaryngology residency were more likely to have been awarded AOA, to have publications, and to have a good Step 1 Score (242 or above). This aligns well with subjective data, as the 2018 survey of program directors showed that success on Step 1 was tied for the most cited factor in the evaluation of a potential candidate. With the variety of data out there, it can be hard to parse out what really matters in an application.
HOW ARE COMPONENTS OF THE APPLICATION WEIGHTED?
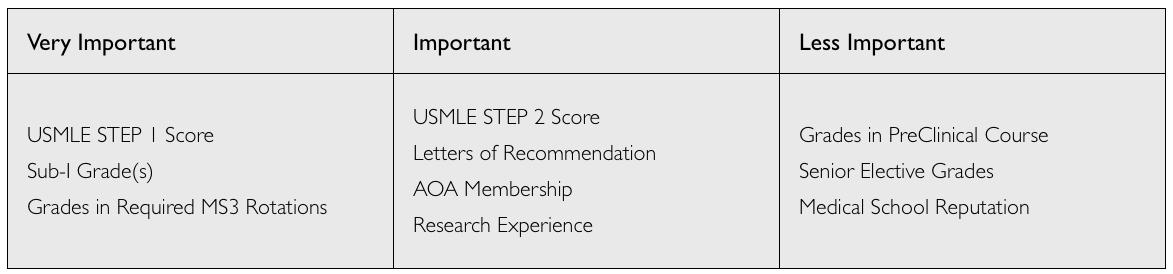
Medical school represents an insanely busy time for most students with more things to do than time to do them. No student will have a flawless application in every area and most applicants do match. Successful applicants are those who are able to prioritize their time to maximally improve their application in the areas that are given the most weight. To give applicants a general sense of how various areas of the application are weighted, we have assigned the main criteria on which applicants are graded into 3 rough categories of importance. Realize that programs will vary in different areas, and not everyone will universally agree on everything, but this table provides a general framework for how different aspects of the application are weighted.
Note: It is important to point out that with the USMLE Step I changes in 2021-2022 there may be a considerably different approach to residency selection. Please look to the end of this page for more information.
GRADES
Applicants should aim at being within the top 3rd of the class. Your first 2 years are vitally important when it comes to setting the foundational backbone of your clinical knowledge. However, while outstanding grades in the first 2 years of medical school are helpful, program committees consider 3rd and 4th year clinical grades to be more predictive of future residency performance.
It is also important to note that with the strong trend of medical schools moving to pass/fail for at least the preclinical years (and possibly for the entire 4 years), the impact of grades may be waning. Couple that with the divergent methods of awarding honors/high pass among the different medical schools and it often becomes very difficult to accurately identify the most successful applicants within a large pool of high-achieving medical students. Studies by Rohe et al. (2006) and Slavin et al. (2014) suggest that a pass/fail schematic for academics allowed for less stress and greater group cohesion among medical students. In summary, evaluating medical school grades may become increasingly complicated in coming years.
Grades within the field (sub-I and visiting rotations) are given the strongest weight, followed closely by grades within certain core rotations such as medicine and surgery. Do not worry if you do not receive honors on every rotation – extremely few applicants achieve honors in every class. Obviously, focus your energy on the rotations that carry the most weight.
As for Alpha Omega Alpha (AOA), like most surgical fields, having this on your application can be helpful for getting noticed by top programs. While AOA membership will by no means guarantee residency placement, it can help get interviews. However, selection committees know that many medical schools do not have AOA chapters and criteria for induction vary from school to school. Therefore, AOA is helpful but not necessary to match at a top program. After all, only about 40-45% of those who match are members.
BOARD SCORES & WHEN TO TAKE STEP 2 CK
Your USMLE Step 1 score is one of the few objective metrics that programs may use to narrow down their application numbers. Make sure that you allocate ample time toward studying for this exam so that you score well. Many, but not all, programs will use arbitrary cut-off scores to help determine who they will invite for an interview -- having a score of 230 or higher will usually make the cut at most places. Remember that your application is a package deal (not just your board score), so if your score is less than the 235-240 average, you should focus on making up for this in other areas of your application. One option is to take Step 2 early enough for it to be added to the application -- and of course, to nail it! If you decide to go this route, you must be confident that you will increase your score by a significant margin. If your USMLE score is already good, it may be risky to take Step 2 early since you have more to lose by scoring poorly.
RESEARCH PRODUCTIVITY
Research is a major aspect of Otolaryngology, both in application and in practice. According to the AAMC, in 2019 PGY1 residents in Otolaryngology had an average number of 11.3 combined abstracts, presentations, and publications. As noted above, applicants with publications under their belt tend to fare better in the application process. Thus, getting involved in research early and often can help your application in more ways than one.
CHANGES TO USMLE STEP 1
On February 12, 2020, the Federation of State Medical Boards (FSMB) and the National Board of Medical Examiners®(NBME®) made a joint agreement about the future of the USMLE Step 1 exam. This includes changing Step 1 from a three-digit score to pass/fail, reducing the allowable number of exam attempts from six to four, and requiring all examinees to pass Step 1 before being allowed to take Step 2 Clinical Skills. These changes are subject to take effect no earlier than January 1, 2022 with further details to follow later this year. Thus, there will likely be a short period of time when some applicants may have scores and others won’t, depending on when students take Step 1. Eventually, all applicants will have moved over to the pass/fail score.
What do the new changes to USMLE Step 1 mean for the applicant? As of now, a lot of what is known about the impact of this decision is conjecture. As noted above, Step 1 was a valuable tool for residency committees to screen prospective candidates and does have a positive correlation with successful residency matches.
Here are a couple of things that these changes could do:
Prioritize Step 2 CK scores. As of right now, Step 2 CK is not a remarkably important tool for Otolaryngology and most surgical subspecialties. In the 2018 survey of program directors, Step 2 was considered an important factor among only 56% of program directors in Otolaryngology. However, with Step 1 becoming pass/fail, the performance on Step 2 CK may end up becoming a new screening tool for residencies.
Increase weight placed on medical school rank and personal networks. This may inherently favor applicants who come from strong home programs. An op-ed from statnews goes into more detail about this, saying, “Without objective standards like standardized testing or grades, residency directors will have to focus on who you know and what you are. Using the who-you-know standard will place even more pressure on students to secure entrance into prestigious colleges and medical schools because the proxy of academic pedigree and network of elite institutions will carry more weight when it comes to placement in residency and fellowship programs.”
One important implication for these changes is that for DO and IMG applicants, this potentially renders your path even more difficult. For non-allopathic applicants and international medical graduates, a past ‘equalizer’ would be to succeed on the Step 1 exam. With this now becoming pass/fail, it could make matching more arduous. An insightful editorial on this topic can be accessed on Kevinmd.com.
Render grades more important. As of right now, grades are certainly being phased out of medical school curricula. However, with these changes, grades could come back into favor.
Render research more important. There is one change to the residency selection process that is almost guaranteed: research productivity. Research productivity has been shown to be positively correlated with successful match into Otolaryngology and even the 2018 program director survey suggested that while just 74% of PDs factor research productivity as an important metric, of those that do, they rate it a 4.0 (out of 5.0). With these changes, it makes sense to assume that research will become even more important. It’s possible that some applicants may preemptively elect to participate in research fellowship years to boost their application.
Conclusion: It is impossible to know the ramifications that will result from the transition of Step 1 to a “pass/fail” test. As this evolves over the coming years, this section will be updated with timely data and information.
RELATED ARTICLES